Learninsta presents the core concepts of Biology with high-quality research papers and topical review articles.
Human Circulatory System
The structure of the heart was described by Raymond de viessens, in 1706. Human heart is made of special type of muscle called the cardiac muscle. It is situated in the thoracic cavity and its apex portion is slightly tilted towards left. It weighs about 300g in an adult. The size of our heart is roughly equal to a closed fist. Heart is divided into four chambers, upper two small auricles or atrium and lower two large ventricles.
The walls of the ventricles are thicker than the auricles due to the presence of papillary muscles. The heart wall is made up of three layers, the outer epicardium, middle myocardium and inner endocardium. The space present between the membranes is called pericardial space and is filled with pericardial fluid.
The two auricles are separated by inter auricular septum and the two ventricles are separated by inter ventricular septum. The separation of chambers avoids mixing of oxygenated and deoxygenated blood. The auricle communicates with the ventricle through an opening called auriculo ventricular aperture which is guarded by the auriculo ventricular valves.
The opening between the right atrium and the right ventricle is guarded by the tricuspid valve (three flaps or cusps), whereas a bicuspid (two flaps or cusps) or mitral valve guards the opening between the left atrium and left ventricle (Figure 7.6). The valves of the heart allows the blood to flow only in one direction, i.e., from the atria to the ventricles and from the ventricles to the pulmonary artery or the aorta.
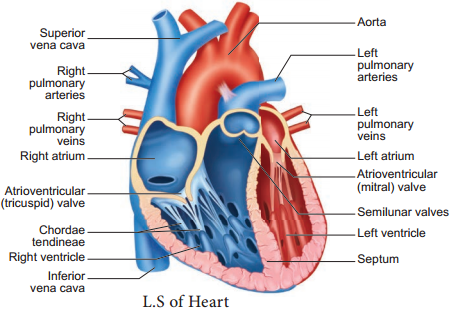
The opening of right and left ventricles into the pulmonary artery and aorta are guarded by aortic and pulmonary valves and are called semilunar valves.
Each semilunar valve is made of three half – moon shaped cusps. The myocardium of the ventricle is thrown into irregular muscular ridges called trabeculae corneae. The trabeculae corneae are modified into chordae tendinae.
The opening and closing of the semilunar valves are achieved by the chordae tendinae. The chordae tendinae are attached to the lower end of the heart by papillary muscles. Heart receives deoxygenated blood from various parts of the body through the inferior venacava and superior venacava which open into the right auricle. Oxygenated blood from lungs is drained into the left auricle through four pulmonary veins.
Origin and Conduction of Heart Beat
The heart in human is myogenic (cardiomyocytes can produce spontaneous rhythmic depolarisation that initiates contractions). The sequence of electrical conduction of heart is shown in Figure 7.7. The cardiac cells with fastest rhythm are called the Pacemaker cells, since they determine the contraction rate of the entire heart.
These cells are located in the right sinuatrial (SA) node / Pacemaker. On the left side of the right atrium is a node called auriculo ventricular node (AV node). Two special cardiac muscle fibres originate from the auriculo ventricular node and are called the bundle of His which runs down into the interventricular septum and the fibres spread into the ventricles. These fibres are called the Purkinje fibres.
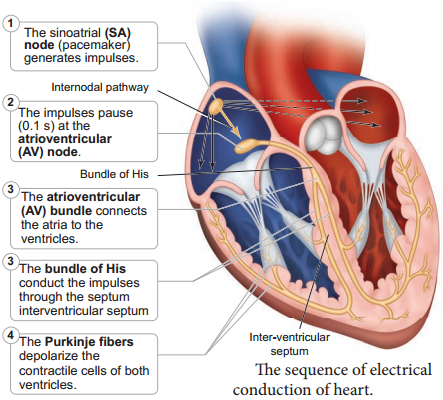
Pacemaker cells produce excitation through depolarisation of their cell membrane. Early depolarisation is slow and takes place by sodium influx and reduction in potassium efflux. Minimum potential is required to activate voltage gated calcium (Ca+) channels that causes rapid depolarisation which results in action potential. The pace maker cells repolarise slowly via K+ efflux.
HEART BEAT:
Rhythmic contraction and expansion of heart is called heart beat. The contraction of the heart is called systole and the relaxation of the heart is called diastole. The heart normally beats 70-72 times per min in a human adult. During each cardiac cycle two sounds are produced that can be heard through a stethoscope.
The first heart sound (lub) is associated with the closure of the tricuspid and bicuspid valves whereas second heart sound (dub) is associated with the closure of the semilunar valves. These sounds are of clinical diagnostic significance. An increased heart rate is called tachycardia and decreased heart rate is called bradycardia.
Cardiac Cycle
The events that occur at the beginning of heart beat and lasts until the beginning of next beat is called cardiac cycle. It lasts for 0.8 seconds. The series of events that takes place in a cardiac cycle.
PHASE 1:
Ventricular Diastole:
The pressure in the auricles increases than that of the ventricular pressure. AV valves are open while the semi lunar valves are closed. Blood flows from the auricles into the ventricles passively.
PHASE 2:
Atrial Systole:
The atria contracts while the ventricles are still relaxed. The contraction of the auricles pushes maximum volume of blood to the ventricles until they reach the end diastolic volume (EDV). EDV is related to the length of the cardiac muscle fibre. More the muscle is stretched, greater the EDV and the stroke volume.
PHASE 3:
Ventricular Systole (isovolumetric contraction):
The ventricular contraction forces the AV valves to close and increases the pressure inside the ventricles. The blood is then pumped from the ventricles into the aorta without change in the size of the muscle fibre length and ventricular chamber volume (isovolumetric contraction).
PHASE 4:
Ventricular Systole (ventricular ejection):
Increased ventricular pressure forces the semilunar valves to open and blood is ejected out of the ventricles without backflow of blood. This point is the end of systolic volume (ESV).
PHASE 5:
(Ventricular Diastole):
The ventricles begins to relax, pressure in the arteries exceeds ventricular pressure, resulting in the closure of the semilunar valves. The heart returns to phase 1 of the cardiac cycle.
Cardiac Output
The amount of blood pumped out by each ventricle per minute is called cardiac output(CO). It is a product of heart rate (HR) and stroke volume (SV). Heart rate or pulse is the number of beats per minute. Pulse pressure = systolic pressure – diastolic pressure.
Stroke volume (SV) is the volume of blood pumped out by one ventricle with each beat. SV depends on ventricular contraction. CO = HR X SV. SV represents the difference between EDV (amount of blood that collects in a ventricle during diastole) and ESV (volume of blood remaining in the ventricle after contraction).
SV = EDV – ESV. According to Frank – Starling law of the heart, the critical factor controlling SV is the degree to which the cardiac muscle cells are stretched just before they contract. The most important factor stretching cardiac muscle is the amount of blood returning to the heart and distending its ventricles, venous return.
During vigorous exercise, SV may double as a result of venous return. Heart’s pumping action normally maintains a balance between cardiac output and venous return. Because the heart is a double pump, each
side can fail independently of the other. If the left side of the heart fails, it results in pulmonary congestion and if the right side fails, it results in peripheral congestion. Frank – Starling effect protects the heart from abnormal increase in blood volume.
Blood Pressure
Blood pressure is the pressure exerted on the surface of blood vessels by the blood. This pressure circulates the blood through arteries, veins and capillaries. There are two types of pressure, the systolic pressure and the diastolic pressure. Systolic pressure is the pressure in the arteries as the chambers of the heart contracts. Diastolic pressure is the pressure in the arteries when the heart chambers relax.
Blood pressure is measured using a sphygmomanometer (BP apparatus). It is expressed as systolic pressure/diastolic pressure. Normal blood pressure in man is about 120/80mm Hg. Mean arterial pressure is a function of cardiac output and resistance in the arterioles.
The primary reflex pathway for homeostatic control of mean arterial pressure is the baroreceptor reflex. The baroreceptor reflex functions every morning when you get out of bed. When you are lying flat the gravitational force is evenly distributed.
When you stand up, gravity causes blood to pool in the lower extremities. The decrease in blood pressure upon standing is known as orthostatic hypotension. Orthostatic reflex normally triggers baroreceptor reflex. This results in increased cardiac output and increased peripheral resistance which together increase the mean arterial pressure.
Electrocardiogram (ECG)
An electrocardiogram (ECG) records the electrical activity of the heart over a period of time using electrodes placed on the skin, arms, legs and chest. It records the changes in electrical potential across the heart during one cardiac cycle. The special flap of muscle which initiates the heart beat is called as sinu-auricular node or SA node in the right atrium.
It spreads as a wave of contraction in the heart. The waves of the ECG are due to depolarization and not due to contraction of the heart. This wave of depolarisation occurs before the beginning of contraction of the cardiac muscle. A normal ECG shows 3 waves designated as P wave, QRS complex and T wave as shown in Figure 7.8 and the stages of the ECG graph are shown in Figure 7.9.
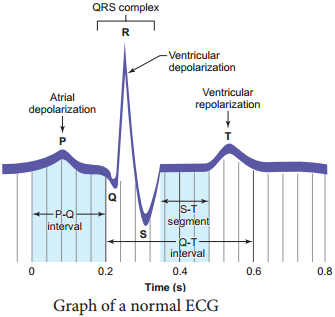
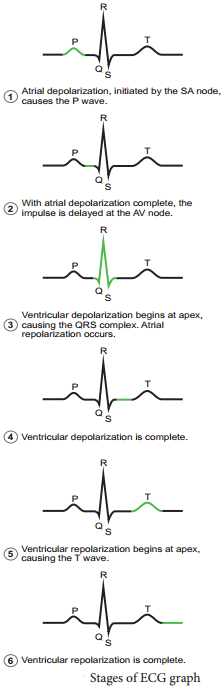
P Wave (Atrial depolarisation)
It is a small upward wave and indicates the depolarisation of the atria. This is the time taken for the excitation to spread through atria from SA node. Contraction of both atria lasts for around 0.8-1.0 sec.
PQ Interval (AV node delay)
It is the onset of P wave to the onset of QRS complex. This is from the start of depolarisation of the atria to the beginning of ventricular depolarisation. It is the time taken for the impulse to travel from the atria to the ventricles (0.12-0.21sec). It is the measure of AV conduction time.
QRS Complex (Ventricular depolarisation)
No separate wave for atrial depolarisation in the ECG is visible. Atrial depolarisation occurs simultaneously with the ventricular depolarisation. The normal QRS complex lasts for 0.06-0.09 sec. QRS complex is shorter than the P wave, because depolarisation spreads through the Purkinjie fires. Prolonged QRS wave indicates delayed conduction through the ventricle, often caused due to ventricular hypertrophy or due to a block in the branches of the bundle of His.
ST Segment
It lies between the QRS complex and T wave. It is the time during which all regions of the ventricles are completely depolarised and reflects the long plateau phase before repolarisation. In the heart muscle, the prolonged depolarisation is due to retardation of K+ efflux and is responsible for the plateau. The ST segment lasts for 0.09 sec.
T Wave (Ventricular repolarisation)
It represents ventricular repolarisation. The duration of the T wave is longer than QRS complex because repolarisation takes place simultaneously throughout the ventricular depolarisation.